New data expose mysterious world of off-exchange health plans
By Harris Meyer
October 24, 2016 - Modern Healthcare
Average premiums
and deductibles for individual and small-group health plans on the Affordable
Care Act exchanges in 2016 were nearly 13% cheaper than for plans sold off the
exchanges, according to new
data from the Robert Wood Johnson Foundation.
The data set, compiled
from information purchased from Vericred, a New York City-based data company
serving the health insurance industry, provides the most detailed look yet at
how the ACA marketplace compares with the off-exchange market, about which much
less is known. HHS recently estimated that 6.9 million Americans have
individual-market plans they bought outside the ACA exchanges, compared with
10.4 million who have exchange plans. Most off-exchange plans have to comply
with the same ACA benefit and guaranteed issue rules as exchange plans.
The data could help policymakers, insurers, researchers and consumers
better understand the full range of options available in the individual and
small-group markets. It also could assist federal and state policymakers
stabilize the struggling Obamacare individual markets, which are experiencing
rising premiums, exiting insurers, and decreasing competition and consumer
choice.
The average silver plan premium on the exchanges across the country was $279
versus $314 for similar plans sold off the exchanges. In the individual
insurance market alone, the average rate for a silver plan for a 27-year-old on
the exchanges was $283 versus $320 off the exchanges. The rate differences could
result from a number of factors, including network size and deductible and
cost-sharing levels.
In the individual exchange market, silver plans
were by far the most common type of product offered—64.9% versus 16.2% bronze
and 12.3% gold. There was greater variety off the exchanges, where 33.7% of
plans offered were silver, 33.1% were bronze, and 21.6% were gold.
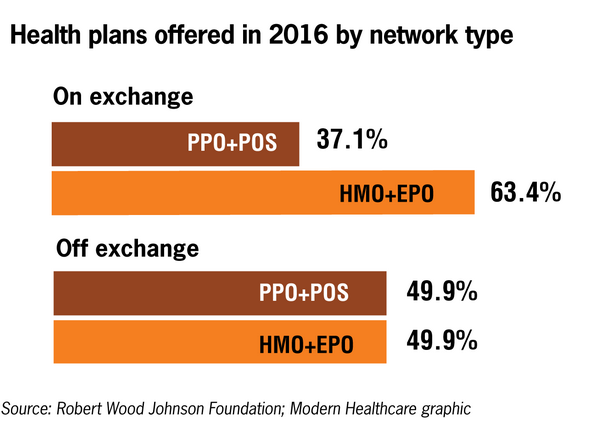
There
also were significant differences in network types offered on and off the
exchanges in 2016, according to the RWJF data. HMO and exclusive provider
organization (EPO) products were far and away the most common products on the
exchanges, making up 63.4% of plans offered compared with 37.1% for preferred
provider organization (PPO) and point-of-service (POS) plans. Off the exchanges,
PPO and POS plans were more common, making up 49.9% of plans offered, the same
percentage as HMO and EPO plans.
Katherine Hempstead, who directs the Robert Wood Johnson Foundation's work on
health coverage, said the data will prove valuable in helping everyone think
about the individual market as a whole. gIt's important for us to understand how
the off-exchange market helps or hinders the exchange market, and whether any
improvement is feasible to organize the two components and make it easier for
consumers to see what's available,h she said.
A number of insurers such
as Aetna are exiting the exchanges in some states while continuing to sell
off-exchange products in those same markets. An Aetna spokesman declined to
discuss details of the company's off-exchange business. But he said Aetna is
maintaining an off-exchange presence to preserve its option under federal law to
re-enter the exchange markets after 2017 gshould there be meaningful
exchange-related policy improvements.h
A Commonwealth
Fund study in June projected that insurers selling only off the exchanges in
2016 spent more on administration and profits and had higher premium increases
compared with insurers that sell mostly on the exchanges.
The new RWJF
data set includes comprehensive information on all individual and small-group
plans offered nationally, including carrier, location, premium, metal tier, type
of plan, and deductible and copayment levels. But it does not include
information on number of plans sold or any information about the people buying
these plans, such as age, income, or health status. While some observers have
speculated that people buying coverage outside the exchanges are healthier and
wealthier than exchange customers, the data don't answer such
questions.
gI hear insurers say the markets are more similar than
different, and I think insurers have lost money in the off-exchange market,h
Hempstead said.
Experts say there are a variety of reasons why consumers
buy coverage outside the exchanges, where they cannot receive an ACA premium
subsidy or cost-sharing reduction. The Obama administration and many experts say
most people in the individual market would be better off buying coverage on the
exchanges because most qualify for subsidies. In contrast, some conservative
analysts favor allowing premium subsidies for coverage purchased outside the
exchanges.
One reason some consumers go off the exchanges is that they
find it simpler to buy a plan directly from an insurer or through a broker if
they think they don't qualify for a subsidy. gIt's easier to move through the
process off the exchange, so convenience is a factor,h said Joel Ario, managing
director of Manatt Health Solutions, who helped establish the federal exchange
as an Obama administration official.
Some customers avoid the exchanges
because they are politically opposed to Obamacare, said Nate Purpura, vice
president of communications for ehealth, an online broker. About half the
261,000 individual plans ehealth sold from October through March were through
the exchanges and about half were off the exchanges.
Consumers looking
for a broader provider network or access to their regular physician or hospital
may have an easier time finding such a plan off the exchange, since PPO and POS
plans are more prevalent outside the exchanges, Hempstead said. Some may be
relatively affluent people who are buying coverage for adult children or other
family members with disabilities or chronic conditions and who want a plan that
gives them access to specialized providers.
Then there are lower-income
consumers who don't realize they can only obtain a premium tax credit through
the ACA exchanges and unwittingly forego that opportunity by buying an
off-exchange plan. HHS estimated this month that 2.5 million consumers who
bought plans off the exchange would be eligible for a subsidy. That includes 1.1
million people with incomes below 250% of the federal poverty level, which
qualifies them for additional cost-sharing subsidies. Another 1.9 million people
who bought off-exchange plans have incomes low enough to qualify for Medicaid.On
top of that, only 52% of uninsured adults were even aware that financial
assistance is available through the ACA exchanges, a recent Commonwealth Fund
survey found. gThere's a huge question about the information status of people
buying off the exchanges,h said Tim Jost, an emeritus law professor at
Washington and Lee University who is an ACA expert.
In addition, Jost
added, some brokers may be steering customers to off-exchange plans because
those plans are more likely to pay a broker fee than exchange plans, which
increasingly do not.
Middle-class consumers who don't qualify for
subsidies may buy outside the exchanges because they are misled or confused.
Michael Anderson, a retired police officer in Scottsdale, Ariz., said he went on
what he thought was the HealthCare.gov federal website to shop for exchange
coverage after he recently retired. But he apparently clicked on copycat
commercial site and got inundated with bogus offers. He ended up buying a
private off-exchange plan through ehealth. The premium, however, is going up
sharply for 2017. So he intends to visit the real HealthCare.gov site in
November to see what's available for him and his wife.
gIt was the first
time I was buying health insurance on my own, and the whole process was very
frustrating,h Anderson said.
Some experts favor merging the exchange and
off-exchange individual markets—which Vermont and Washington, D.C. already have
done—to help stabilize the ACA marketplaces and make it easier for consumers to
shop and compare premiums, benefits and provider networks across all available
individual-market products. Insurers strongly oppose this approach.
gIf
you set up an environment where customers get to compare all prices and products
in one place, that creates true competition and means better prices, and it can
actually reward insurers that provide the best products,h said Mila Kofman,
executive director of the D.C. exchange.
Ario said the new RWJF data
raise more questions than they answer about what's happening in the murky
off-exchange market and how it affects the ACA exchanges. Much more needs to be
known to guide policy and improve the functioning of the entire individual
market, and the data set is a good start.
gUltimately, it's good for
people to have lots of choices for subsidized and unsubsidized products,h he
said. gConsumers should have the same level of transparency about both markets.h